Podcast: Play in new window | Download (Duration: 45:36 — 62.6MB)
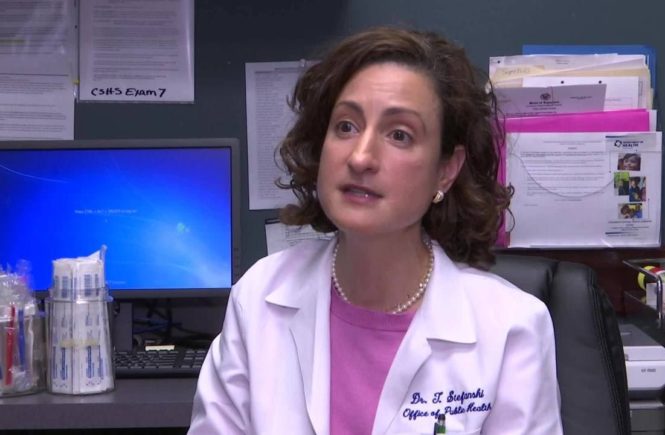
Dr. Tina Stefanski, Medical Director of the Office of Public Health in Acadiana, joined Jan Swift to discuss the current COVID-19 situation in the region. Dr. Stefanski oversees the seven parish region of Acadiana for the Department of Health in all matters relating to maintaining and protecting the health of our citizens.
A graduate of the LSU School of Medicine, Dr. Stefanski completed her pediatric residency program at LSU School of Medicine’s Medical Clinic and Children’s Hospital in New Orleans. A stint on a Public Health rotation ignited her interest in the field and she joined the Louisiana Department of Health immediately after she finished her residency requirements.
The Louisiana Department of Health is involved in all things relating to personal, preventative, and environmental health concerns. Overseeing matters as diverse as ensuring safe drinking water, mental health concerns, working with safety inspectors of restaurants, and preventative health measures such as containing the spread of COVID-19, Dr. Stefanski enjoys the scope of her work and the positive impact it has on our region’s health.
She speaks highly of our “very coordinated medical community” who proactively work together to share information and resources when the need arises. One such group that is active now is the Physicians’ Leadership Counsel co-chaired by Dr. Andy Blalock and Dr. Steve Reese and includes among its members Dr. Chuck Burnell (Acadian Companies), Dr. Ben Doga (Chief Medical Advisor of LHC Group), Dr. Rod Clark (State Board of Medical Examiners), Dr. Anu Desai (President of the Lafayette Parish Medical Society), and chief medical officers of all area hospitals. This working physician’s group discusses best practices and treatments to date on COVID, availability of beds, and other information which will benefit healthcare providers and patients in the region.
In the video below, Dr. Henry Kaufman, Chief Medical Officer of Our Lady of Lourdes, and Dr. Amanda Logue, Chief Medical Officer of Lafayette General Health discuss the spike in pandemic cases, rampant community spread after Phase II rolled out, and the tremendous growth in the number of cases in the 18 to 29 year age group. Both physicians urged the public to wear masks as a way to contain the spread of the virus, slow down the number of hospitalized victims, and be able to get to Phase III to see businesses reopen safely and get back to “normal.”
Dr. Stefanski’s message is premised upon the fact that “no one knows what to predict….there is no way to predict what course this pandemic will take. We’re all learning together. We’ve got to listen to the experts so that we can contain the rate of growth.” She further stressed, however, “There is no mixed message as to what needs to be done to contain the spread of the virus. Every credible medical expert in the country has consistently shared the same message as to the importance of social distancing, good hygiene practices, and wearing a mask. The virus is real. Yet the message is not sticking.”

“There is no mixed message. We all know now how the virus spreads. Every credible medical expert throughout the country has consistently shared the same message as to the importance of social distancing, good hygiene practices, and wearing a mask. The virus is real. Yet the message is not sticking.”
It was initially thought that only symptomatic people would spread the virus, because that is how SARS spread. Now the medical community knows differently. 95 to 96% of cases are coming from community spread, from others who are out and about. When social distancing isn’t possible, it is best practices to wear a mask, don’t touch your face, and be aware of your surroundings.
Dr. Stefanski shared that the 18 to 21-year-old group is the most problematic sector of young people contracting the virus. They are generally not sick like older adults, typically experiencing only mild flu-like symptoms. The concern is that a wave of cases is continuing to build and it will spill over into the 70-year-old and above cohort who come into contact with these young people. These older individuals have seen a decrease in cases as of late because they’ve isolated and been careful. But “they need to be able to get out and shop too….please wear a mask,” urges Dr. Stefanski.
Deaths in the minority community, especially Blacks, are unfortunately still a disproportionate share of COVID victims. Many are over 65 with high blood pressure, diabetes and other underlying health conditions.
The majority of those hospitalized are 55 and up, and 65 and up in the ICU’s. The Acadiana area is in decent shape insofar as available hospital beds, both on the hospital floors and ICU’s.
Dr. Stefanski recounts the problem of seeing young people (or any age for that matter) meet up in small groups of 9 to 10 people as establishments have opened up and people are looser with their conduct….people who don’t normally see one another, coming from different backgrounds, where you don’t know who they’ve been around. It is becoming prevalent to learn after these get-togethers that someone has the virus, causing the whole group to self-quarantine and hope that they don’t contract the virus. “It’s just not a good idea to mix unless you’ll be outside, six feet apart from one another, and preferably wearing a mask. Think through your scenarios…..spending two to three hours inside over dinner is just not a good idea. It seems like people are partying like its 1999!”
If a person at work is diagnosed with the virus, it is not necessarily necessary to self-quarantine. If you have been in close proximity with them for 15 minutes or more you should quarantine, as the level of risk is too high that you may expose others. If your office place is large and you have little to no contact with the person who has the virus, you do not need to be concerned.
It is increasingly problematic to obtain a COVID test if you’re asymptomatic due to a shortage of tests. And, results can take ten to twelve days to get back. Dr. Stefanski says if you are symptomatic you should be able to be tested. In any event, if you’ve been exposed, the best action is to stay home and quarantine. Even if you take a test that comes back negative, you still must quarantine as the virus may not have manifested yet. The incubation process varies and some people develop symptoms in two to five days, others may take 13 to 14 days before symptoms appear.
People may test positive for four, five or even six weeks after their illness subsides. It is important to note, however, that the virus is no longer ‘live’ after 10 days, even in a person who continues to test positive. The CDC has documented that it has not been able to successfully culture the virus more than 9 days after onset of illness and you’re not likely to be contagious. Dr. Stefanski counseled, “If my symptoms start today, I start counting tomorrow as Day One. Count 10 days, and once you’re in the tenth day you are unlikely to prove contagious.” There is a caveat to workers in nursing homes, prison, and other close quarters to wait up to 14 days before returning to work.
The homeless population in the region has fared exceptionally well, much better than other areas of the country. Our Homeless Coalition non-profits have worked tirelessly to prevent the spread. This is also true with the local jail population.
It is important to answer calls from the Louisiana Department of Health as they employ contact tracers who track down who may have been exposed and alert others to their risk. The Department will be identified on your phone and answering their call is a public service….to yourself and others.
Dr. Stefanski wanted to clarify one last point on the issue of how the Department of Health reports the ‘case count.” Each individual case is counted only once in the state’s official COVID tally, even if that individual has taken multiple tests that prove positive. In other words, it is based upon the individual case, not the number of tests associated with that case. (The Department has had to revise official counts to ensure there was no duplication and the varying numbers have raised questions as to accuracy.)
Discover Lafayette would like to thank Dr. Tina Stefanski for her commitment to public health and her dedication to our community. For more information and the latest updates from the Louisiana Department of Health, visit http://ldh.la.gov/.